At My Surgical Specialist, we are at the cutting edge of gastric cancer (stomach cancer) treatment. The team approach from our experts ensures that you receive the most up-to-date and comprehensive treatment, personalised to your situation. Mr Alkhaffaf and his team will take the time to answer all your questions and help you make the right decisions about your care.
Common Questions About Stomach (Gastric) Cancer
Q: What is the Stomach?
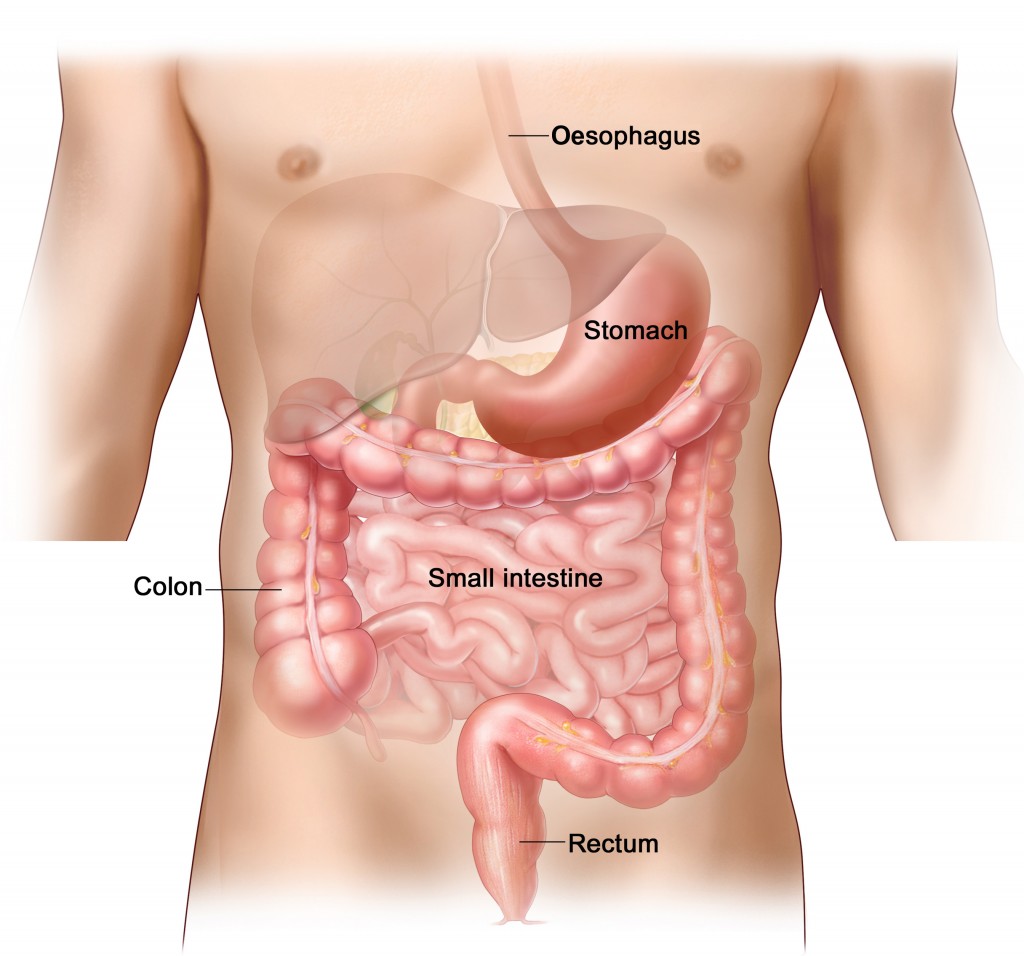
The stomach is a muscular ‘bag’ which helps digest the food and drink that we swallow. It is found in the upper abdomen.
Q: What is Gastric Cancer (Stomach Cancer)?
This is a potentially life-threatening abnormal growth which occurs in the stomach and usually starts from the inner lining. The commonest type of stomach cancer is ‘adenocarcinoma’. Other cancer-like tumours which grow in the stomach include ‘neuro-endocrine tumours’ and ‘gastro-intestinal stromal tumours’ (GIST).
Q: How Common is Stomach Cancer?
Gastric cancer is not as common as it once was. However, approximately 7000 new cases are diagnosed each year in the UK.
Q: What Are the Symptoms?
Gastric cancer can cause a range of symptoms or problems, the commonest being:
-Sensation of food sticking when you swallow
–Vomiting and nausea
–Pain in the abdomen
–Indigestion or heartburn which is not relieved by medication
-An unexplained loss of weight
-An unexplained loss of appetite
–Tiredness and anaemia
Some of the early signs of gastric cancer are non-specific and are often put down to other common or simple conditions. This can mean that by the time a diagnosis is made, gastric cancer is no longer in its early stages.
Q: What Causes Gastric Cancer?
The exact cause of cancer is not known, however there are a number of factors which can increase your risk of developing gastric cancer. These include:
-Bacterial infection with an organism called ‘helicobacter pylori’
-A history of gastric cancer in your immediate family
-Obesity
-Smoking
-Excessive alcohol consumption
-Previous surgery to remove part of your stomach
Q: What is the Prognosis?
The prognosis of gastric cancer depends on many factors, the most important being how advanced the tumour is when it is diagnosed (tumour stage). The earlier the diagnosis is made, the better the prognosis.
Mr Alkhaffaf and his team of experts will talk to you about these factors in detail and will ensure that you are given the correct information specific to your particular situation.
Q: How is Stomach Cancer Treated?
The treatment of gastric cancer depends of many factors such as how early the cancer is (stage of cancer) and your general health and fitness. More often than not, treatment which is given with the intention of curing gastric cancer involves a combination of chemotherapy and surgery to remove part or all of your stomach.
Mr Alkhaffaf will talk to you about the right treatment for you. They will walk you through the entire process so that you can make the right decisions about your treatment.
Q: How Successful is Surgery for Acid Reflux?
Anti-reflux surgery is a well established treatment and as such there is a wealth of information on its long-term success. Advances in surgery such as keyhole (laparoscopic) techniques have significantly improved results after surgery. Approximately 9 out of 10 patients achieve long-term satisfaction following their surgery and would recommend it as a treatment to someone who has GORD.
A small number of patients (approximately 20%) find that although symptoms of reflux are significantly reduced, they still need to take anti-acid medication – albeit often at a lower dose than they did previously.
Q: Are There Any Risks With Surgery?
Keyhole anti-reflux surgery is safe and effective and the risks associated with it are small. However no procedure or surgery is risk-free. Complications in the immediate post-operative period can include:
–Internal bleeding: In some cases where the hiatus hernia is particularly large, your surgeon may temporarily place a drain tube (a small tube which comes out of the abdomen) at the site of surgery for 24 hours to ensure that there is no bleeding following the procedure. This may delay your hospital discharge.
–Infection of the keyhole wounds
–Perforation: The keyhole instruments used during surgery can injure surrounding structures, such as the intestine, bowel and blood vessels. This type of injury is extremely rare, occurring in less than 1% of cases, and can usually be repaired at the time of the operation.
–DVT: A ‘deep vein thrombosis’ is another word for a clot in the leg. These clots can rarely also travel to the lung. We routinely prescribe you special stockings and blood thinning medication following your surgery to reduce the risk of this happening. In addition, because keyhole surgery enables you to return to your daily activities quickly, the risk of developing a DVT is further reduced.
–Difficulty Swallowing: this can occur immediately following surgery usually because of swelling around the bottom of the oesophagus. It is important to follow our special post-operative diet to reduce the risk of this problem whilst the healing process takes place and the swelling in the area settles naturally.
Some of the longer-term problems which may occur include:
–Bloating: A degree of bloating can occur following surgery. The stomach wrap reduces acid reflux from the stomach into the oesophagus. As a result, the wrap also can reduce the amount of gas that you naturally bring up (burping) and can lead to bloating.
–Dumping syndrome: This is a collection of symptoms including diarrhoea, abdominal cramps, sweating, dizziness, headaches and fatigue which can occur after gastric bypass surgery. Some patients complain of dumping syndrome to varying degrees.
–Failure of procedure: Treatment failure occurs in approximately 1 in 10 patients and requires careful investigation to identify its cause.